Probiotics as adjuvant therapy for COVID-19 patients
"In COVID-19 patients, probiotics could help to restore the altered gut microbiota, contributing to a healthy gut-lung axis."
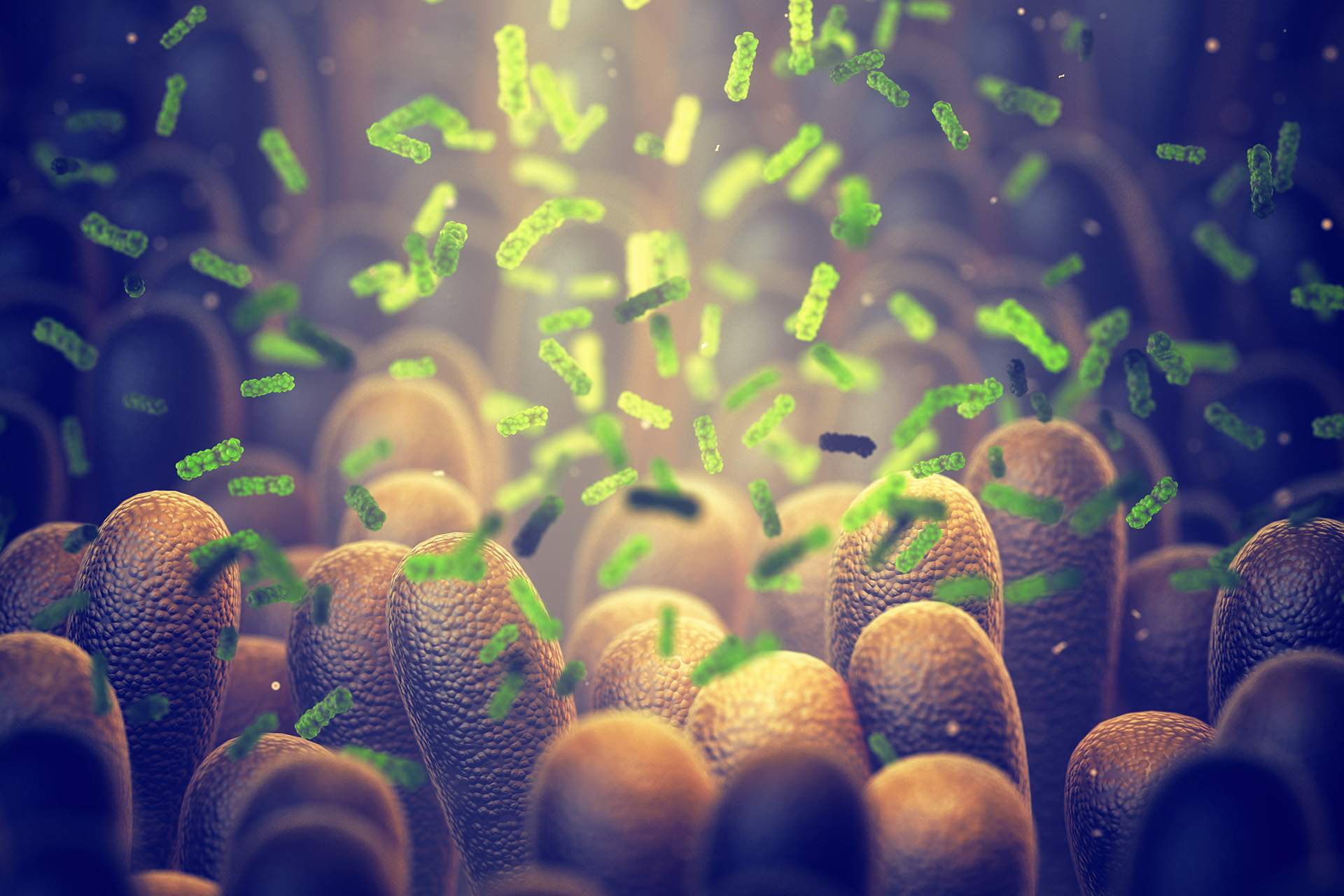
SARS-CoV-2's action on microbiota
The most frequent symptoms of SARS-CoV-2 infection are fever, body aches, nasal congestion, dry cough, and sore throat. However, about 5-10% of patients suffer from gastrointestinal symptoms, such as nausea, vomiting, diarrhea, and abdominal pain.
Other less frequent symptoms are total or partial loss of the sense of smell/taste, neurological symptoms, cerebrovascular events, neuropsychiatric symptoms and skin manifestations.
Based on the observed symptoms, one can hypothesize that SARS-CoV-2 interacts with the gut microbiota via the gut/lung axis. The authors believe it could also be responsible for neuropsychiatric and cutaneous manifestations through the gut/brain and gut/ skin, and skin/brain axes.
With the viral entry into the host cell, leading to lung damage and the subsequent series of reactions that end in an altered expression of antimicrobial peptides on Paneth’s intestinal cells – an alteration that modifies the composition of the intestinal microbiota. Thus evidently influencing the gut/lung crosstalk.
Notably, SARS-CoV-2 infected patients are often administered antibiotics and antivirals, which could also result in further gut microbiota dysbiosis.
In this context, the authors report several studies where the intestinal microbiome presented bacterial diversity in SARS-CoV-2 cases – correlating directly or inversely. This kind of bidirectional link is also observed between the intestinal microbiota and the skin. A SARS-Cov-2 patient manifesting skin symptoms may have alterations of the gut microbiota – that partly justify their presence to the immune process of gut/skin crosstalk.
SARS-CoV-2 infection and the role of probiotics in microbiota dysbiosis
It is well established that probiotics strengthen and modulate the immune system, contribute to repopulating the gut with “good” bacteria, hinder pathogen proliferation, and help to establish a condition of eubiosis (microbial balance in the body).
The term probiotics include many species, such as Lactobacillus spp., Bifidobacterium spp, Enterococcus spp, and Saccharomyces spp, Leuconostoc, Pediococcus. The Lactobacillus spp. (L. rhamnosus) and Bifidobacterium spp. (B. lactis HN019) are commonly in fermented products, such as yogurts and cheeses.
Based on this study’s rationale, the authors note it is recommendable to use probiotics, and their metabolites SCFAs (short-chain fatty acids), to reinforce innate and adaptive immunity in SARS-CoV-2 patients. It can be an adjuvant strategy against complications.
The administration of probiotics is observed to increase anti-inflammatory cytokines, decrease pro-inflammatory cytokines, improve antiviral antibody production, and reduce the viral load. Taking probiotics has immensely improved the condition of the clinical patient, too, in many cases. These observations indicate that the probiotics would be useful in reducing SARS-CoV-2 dissemination in the respiratory tract and gut, reinforcing both anti-inflammatory responses and immune defenses.
Conclusion:
In summary, this review aims to focus on current knowledge about the use of probiotics as adjuvant therapy for COVID-19 patients. The probiotics seem effective in lowering inflammatory status, moreover in patients with chronic comorbidities such as cancer and diabetes, improving clinical outcomes, the team concludes.
Article Source:
News Medical Life Science.
https://www.news-medical.net/?tag=/Probiotics